
November is Diabetic Eye Disease Awareness Month. This is a good time for the doctors at Minnesota Eye Consultants to help our patients learn about how diabetes can affect your eyes, and what proactive steps you can take to protect your vision.
Many people with diabetes can live long and healthy lives. But the longer that you have diabetes and poorly controlled blood sugar levels, the higher your risk of developing diabetic eye disease. This is the leading cause of blindness in adults between 20 and 65 years of age.
The good news is that most diabetic eye problems can be controlled. The key to managing diabetes and avoiding complications is through diet, exercise, taking prescribed medications, and not smoking.
You can protect your vision with a combination of a healthy lifestyle and early detection and treatment of any eye problems.
In early diabetes, high blood sugar can cause the lens of the eye to swell. Often the first symptom that diabetics may experience is blurry vision.
Once blood sugar levels are under control, it can take up to 3 months for vision to seem normal again. As diabetes progresses, several different types of eye disease can develop:
Cataracts
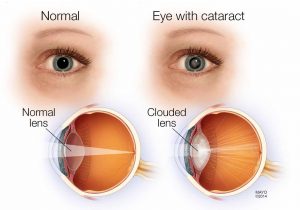
Cataracts can be caused by excess blood sugar. A cataract is a clouding of the lens of the eye, which makes the lens unable to focus.
Diabetics are more likely to develop cataracts than other people, and they often get them at an earlier age. Cataracts are treated with surgery, in which the cloudy lens is removed and replaced with a clear lens.
Glaucoma
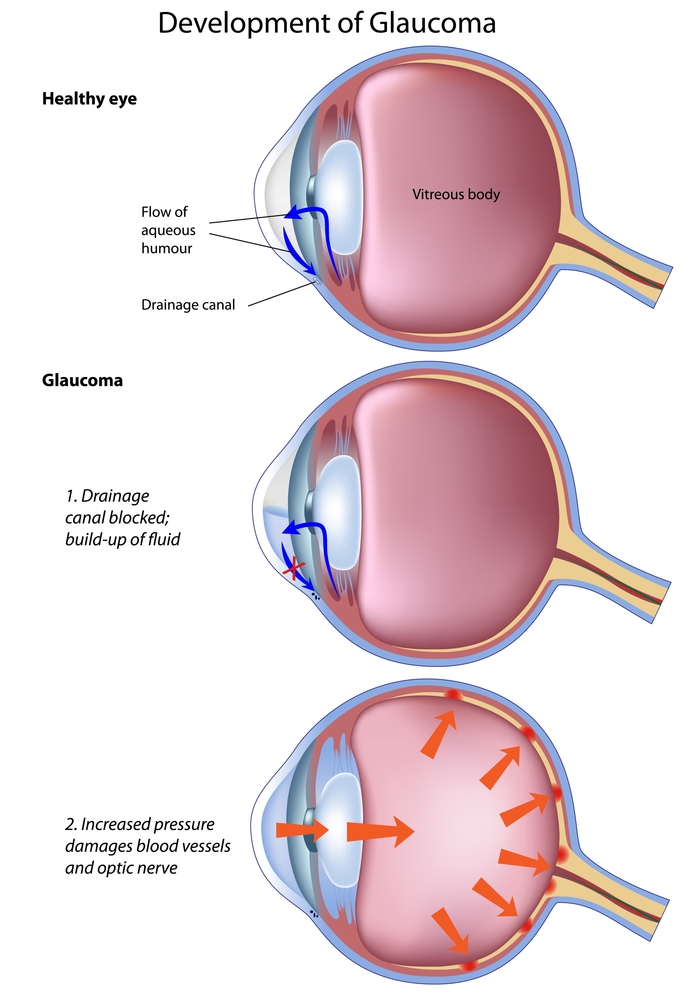
Glaucoma is a group of diseases that damage the optic nerve, which connects the eye to the brain. Diabetics are twice as likely as other people to develop glaucoma.
There aren’t many early symptoms, so many patients are not aware they have glaucoma until their peripheral (side) vision has been severely damaged. Most types of this disease are caused by elevated pressure inside the eye.
People with diabetes can develop neovascular glaucoma, in which new blood vessels grow into the iris and causes eye pressure to elevate. Glaucoma can be treated with eye drops to control pressure, laser treatments, and surgery.
Diabetic Retinopathy
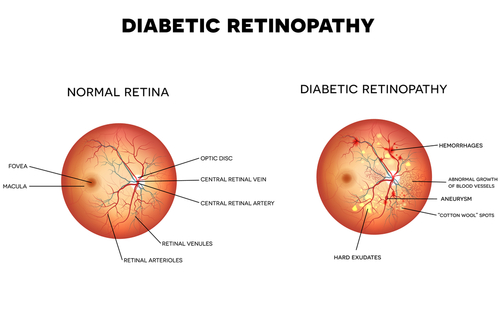
Diabetic retinopathy is the most common eye disease that affects diabetics. At first, patients may not experience any vision changes or pain, even though the damage is occurring inside the eye.
High blood sugar can damage the tiny blood vessels in the retina, which is a nerve layer at the back of your eye that relays images to your brain. It causes blood vessels in the retina to weaken and leak fluid.
There are four stages of diabetic retinopathy, which simply means damage to the retina. As the disease progresses, some blood vessels become blocked and interfere with the blood supply to the retina.
In the most advanced stage, which is called proliferative retinopathy, the retina triggers the development of abnormal new blood vessels to grow (or proliferate) on the surface of the retina. These blood cells can rupture and bleed, causing hemorrhages in the retina and vitreous gel lining.
Scar tissue may grow and tug at the retina, causing a dangerous condition called retinal detachment.
Diabetic retinopathy can seriously impair vision if not detected and treated. The good news is that some effective treatments have been developed in recent years, including lasers that stop bleeding, and anti-VEGF injections into the eye.
Anti-VEGF treatments can stop vision loss and may actually improve vision in some people.
Diabetic Macular Edema
Diabetic macular edema is actually a consequence of diabetic retinopathy. It occurs when retinal blood vessels leak into the macula, which is the part of the retina that helps us see fine detail and color.
These leakages cause the macula to thick and swell, and eventually distort the central vision. It is also treated with anti-VEGF injections.
What Can You Do To Protect Vision As A Diabetic?
If you have diabetes, there are many steps that you can take to protect your eyes from vision loss. Focus on these four key steps to achieve better diabetic health: managing your A1C, controlling your blood pressure, lowering your cholesterol, and quitting smoking.
The most important thing that you can do to preserve healthy vision is to control your blood sugar. Your doctor will recommend the target blood sugar range that you should maintain using a healthy diet and medications. High blood pressure often accompanies diabetes and needs to be controlled as well.
There are some symptoms of diabetic eye disease that you should watch out for, such as blurry or wavy vision, frequent changes in vision, dark areas in the vision, poor color vision, floaters (spots or strings) and flashes of light. You should always call your eye doctor right away if you experience sudden changes in vision or flashes of light.
This can be a symptom of a detached retina and should be treated as soon as possible.
It is important not to assume that your eyes are healthy because your vision seems ok and you haven’t noticed any symptoms. Having a comprehensive eye exam at least once a year is another important way of maintaining healthy vision.
An eye exam that only checks your near and far vision may not detect early diabetic eye disease. Your ophthalmologist or optometrist will need to dilate your eyes to see the retina and optic nerve at the back of the eye.
Dilation is performed by inserting some drops in your eyes that temporarily widen the pupils. Checking eye pressure is another critical part of a comprehensive exam, as high pressure can be a sign of glaucoma.
Annual eye exams help your eye doctor find and treat problems early. If you have already been diagnosed with diabetic eye disease, your eye care provider may recommend more frequent checkups.
Early treatment of diabetic eye disease will be much more effective than waiting until vision loss has progressed. It’s never too late to take better care of yourself and your vision!
Have questions about diabetic eye disease? Schedule an appointment with the experts at Minnesota Eye Consultants in Minneapolis, MN!









